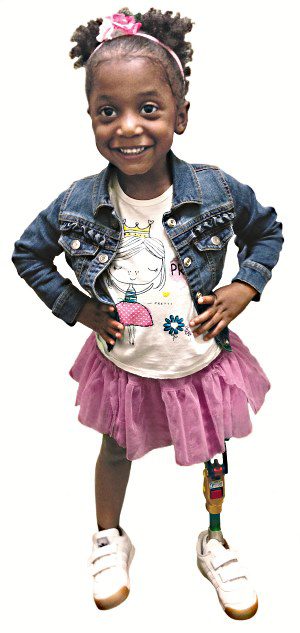
Over the years, the Prosthetic Industry has made significant advancements in designs, components, materials and processes. The increase in comfort and functionality of prosthetics these days is outstanding…as long as you are over the age of 12 that is. What has lagged behind is the entire field of pediatric prosthetics for young children – who …

As many of you know, this past year EastPoint became the first clinical partner with LIM Innovations, out of San Francisco, California. In September of 2014, LIM released a revolutionary new socket design, a game-changer in the prosthetic world, the Infinite Socket. The Infinite Socket is the first of its kind to offer a completely …
Google “skull deformity helmets” and nearly half of the results on the first page are articles that criticize helmet therapy for infants, claiming that the expensive orthotics are a total waste of money. Despite numerous studies that support the effectiveness of helmet therapy in correcting plagiocephaly and brachycephaly [3-6], media sources such as …
Phantom limb pain (PLP) is reported in nearly 80% of patients with missing limbs, yet the causes are still not fully understood. Recent research on the topic has helped to increase our knowledge of PLP, but the varying nature of the condition makes it difficult to define and treat. Patients often experience different sensations described …
